Viral Etiology Relationship between Human Papillomavirus and Human Breast Cancer and Target of Gene Therapy
YAN Chen, TENG Zhi Ping, CHEN Yun Xin, SHEN Dan Hua, LI Jin Tao, and ZENG Yi,,#. State Key Laboratory of Infectious Disease Prevention and Control, National Institute for Viral Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Collabrative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Beijing 0005, China; . Peking University People's Hospital, Beijing 00044, China; . College of Life Science and Bio-engineering, Beijing University of Technology, Beijing 004,China
Original Article
Viral Etiology Relationship between Human Papillomavirus and Human Breast Cancer and Target of Gene Therapy
YAN Chen1, TENG Zhi Ping1, CHEN Yun Xin2, SHEN Dan Hua2, LI Jin Tao3, and ZENG Yi1,3,#
1. State Key Laboratory of Infectious Disease Prevention and Control, National Institute for Viral Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Collabrative Innovation Center for Diagnosis and Treatment of Infectious Diseases, Beijing 100052, China; 2. Peking University People's Hospital, Beijing 100044, China; 3. College of Life Science and Bio-engineering, Beijing University of Technology, Beijing 100124,China
Abstract
Objective To explore the viral etiology of human breast cancer to determine whether there are novel molecular targets for gene therapy of breast cancer and provide evidence for the research of gene therapy and vaccine development for breast cancer.
Methods PCR was used to screen HPV16 and HPV18 oncogenes E6 and E7 in the SKBR3 cell line and in 76 paraffin embedded breast cancer tissue samples. RNA interference was used to knock down the expression of HPV18 E6 and E7 in SKBR3 cells, then the changes in the expression of cell-cycle related proteins, cell viability, colony formation, metastasis, and cell cycle progression were determined.
Results HPV18 oncogenes E6 and E7 were amplified and sequenced from the SKBR3 cells. Of the patient samples, 6.58% and 23.68% were tested to be positive for HPV18 E6 and HPV18 E7. In the cell culture models, the knockdown of HPV18 E6 and E7 inhibited the proliferation, metastasis, and cell cycle progression of SKBR3 cell. The knockdown also clearly affected the expression levels of cell cycle related proteins.
Conclusion HPV was a contributor to virus caused human breast cancer, suggesting that the oncogenes in HPV were potential targets for gene therapy of breast cancer.
Human papillomavirus; Human breast cancer; RNA interference; Gene therapy
www.besjournal.com (full text) CN: 11-2816/Q Copyright ©2016 by China CDC
INTRODUCTION
In 2014, breast cancer was estimated to be the second most common cause of death (15%) and the leading cause of new cancer diagnoses (29%) among women[1]. There are many theories about the causes of breast cancer[2-3],including human papillomavirus (HPV)[4-5]. The relationship between HPV and many kinds of cancers, such as cervical carcinoma and head-neck carcinoma,is well established[6-8]. The hypothesis that HPVs might contribute to human breast cancer is based on the immortalization of primary mammary epithelial cells by high-risk HPV. However, there are conflicting reports regarding the prevalence of HPV DNA in breast cancer in different countries[9-14]. Similarly,there are conflicting reports regarding the presence of an HPV18 oncogene in the SKBR3 breast cancercell line[5,15].
Gene therapy is a novel research field and over 63% of gene therapy clinical trials are conducted for cancer treatment. RNA interference (RNAi) is a mechanism of post-transcriptional gene silencing in plants and animals[16-17]. The use of short hairpin RNA (shRNA) to inhibit the expression of defined target genes has cleared therapeutic potential. In the context of breast cancer, identifying a putative target gene is the foundation of efficient gene therapy.
In this study, we aimed to determine whether the E6 and E7 oncogenes from HPV16 and HPV18 contribute to the viral etiology of breast cancer in the SKBR3 cell line and primary breast cancer tissue samples. We then explored whether they are novel viral targets for gene therapy for breast cancer,providing evidence for the future research in gene therapy and vaccine development.
MATERIALS AND METHODS
Human Specimens and Cell Culture
Seventy-six paraffin-embedded breast cancer samples were obtained from Peking University People's Hospital. Of the patients included, 31.58% (24/76) were aged 25-45 years, 50.00% (38/76) were aged 46-65 years, 17.11% (13/76) were aged 66-85 years, and 1.32% (1/76) were aged ≥86 years. In terms of the sex distribution, 1.32% (1/76) were males and 98.68% (75/76) were females. Invasive ductal carcinoma was detected in 98.68% (75/76) of the samples, while invasive lobular carcinoma was detected in 1 (1/76) sample. Of the 75 invasive ductal carcinoma samples, 48.00% (36/75) were in stage I, 34.67% (26/75) were in stage II, and 17.33% (13/75) were in stage III. Written consent statements were obtained from all the patients before the study. This study was carried out in accordance with the Code of Ethics of the World Medical Association. The privacy rights of the human subjects were protected. Human breast cancer cells (SKBR3) and human embryonic kidney (HEK) 293 cell lines were obtained from the Cell Resource Center, Peking Union Medical College. The cell line was confirmed free from mycoplasma contamination by PCR and culture assays. The species origin of the cells was confirmed by PCR. The identity of the cell line was authenticated with STR profiling (FBI, CODIS). HEK293 cells were maintained in Dulbecco's Modified Eagle Media (HyClone, Utah, USA) supplemented with 10% FBS (Gibco, Massachusetts,USA) at 37 °C and 5% CO2. The SKBR3 cells were maintained in 1640 (HyClone, Utah, USA)supplemented with 10% FBS (Gibco, Massachusetts,USA) at 37 °C and 5% CO2.
Detection of HPV Oncogenes in SKBR3 Cells and Breast Cancer Tissue Samples
Detection of HPV Oncogenes in SKBR3 Cells Specific primers (Table 1) were designed based on the mRNA sequence of HPV18 E6, HPV18 E7. The total RNA was extracted from the SKBR3 cells by using Trizol (Invitrogen, Massachusetts, USA). Briefly,each sample was dissolved in 1 mL of Trizol and 0.2 mL of chloroform was added. Then the tube was shaken vigorously for 15 s and centrifuged at 12,000 × g for 15 min. The RNA was extracted by washing the pellet with 1 mL of ice-cold isopropanol followed by cold 75% diethylpyrocarbonate (DEPC) treated ethanol. The ethanol was removed and the tube was briefly air dried. The RNA pellet was resuspended in nuclease-free water. The complementary DNA (cDNA) was synthesized from the total RNA by using the Goscript reverse transcription system (Promega,Wisconsin, USA). The total DNA was extracted by using the QIAamp DNA Blood Mini Kit (Qiagen,Dusseldorf, Germany) from 1×106cells.
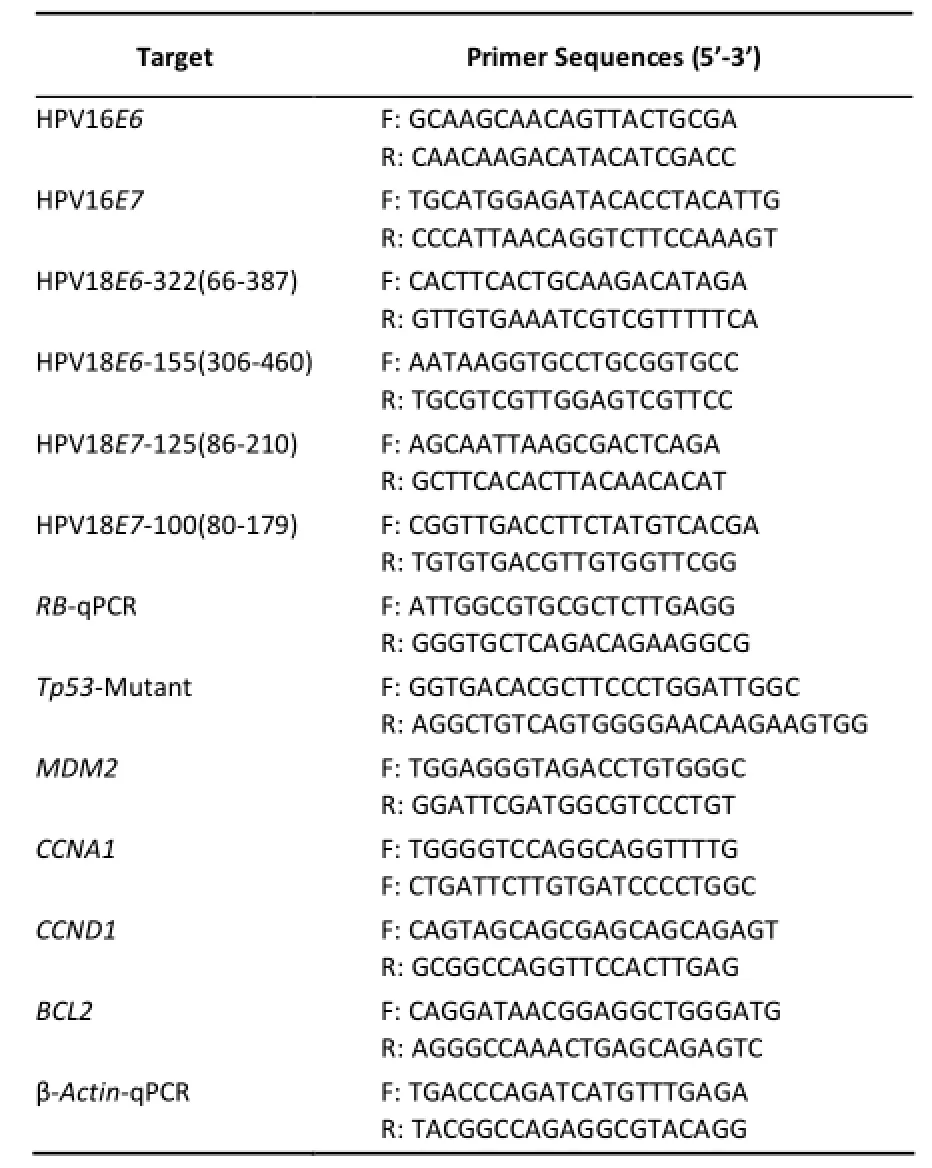
Table 1. Primer Sequences
The cDNA from the SKBR3 cells was used to amplify HPV16E6, HPV16E7, HPV18E6-155 (306-460),and HPV18E7-125 (86-210) by using PrimeSTAR HS (TaKaRa, Dalian, China). The PCR reaction conditions were 30 cycles of 98 °C for 10 s, 59 °C for 15 s, and 72 °C for 10 s. Based on the results, the HPV18E7-125 (86-210) primer was optimized to HPV18E7-100 (80-179). The total DNA from the SKBR3 cells was amplified by using the HPV18E7-100 (80-179) primer. The PCR conditions for this reaction were 30 cycles at 98 °C for 10 s, 55 °C for 15 s, and 72 °C for 10 s. To add the poly-A tail after the PCR reaction, 1 µL of ExTaq (TaKaRa, Dalian, China) was added to the PCR reaction and the mixture was maintained 72 °C for 30 min. Following the amplification, the PCR products were cloned into a T-vector and sequenced.
Detection of HPV Oncogenes in Paraffin-embedded Breast Cancer Samples DNA was extracted from 76 paraffin-embedded breast cancer samples. Briefly,the samples were deparaffinized by placing them in 1 mL of TES (10 mmol/L Tris-Hcl, 1 mmol/L EDTA,and 0.5% SDS) in a 60 °C water bath for 30 min and then centrifuged at 8000 × g for 10 min. The precipitates were dissolved in 500 µL of TET (100 mmol/L Tris-Hcl, 1 mmol/L EDTA, 1% TrisonX-100,and 500 µg/mL Proteinase K) in a 60 °C water bath for 1 h. The mixture was purified with hydroxybenzene-chloroform-Isoamyl alcohol, and then NaAc (3 mol/L) and alcohol were added to precipitate the DNA. The DNA pellet was resuspended in nuclease-free water.
Dual-PCR was used to determine whether HPV oncogenes are detectable in the breast cancer samples by using primers for HPV16E6, HPV16E7,HPV18E6-322 (66-387), HPV18E7-100 (80-179) and ExTaq (TaKaRa, Dalian, China). The reaction conditions were 94 °C for 2 min; 30 cycles at 94 °C for 30 s, 55 °C for 30 s, and 72 °C for 1 min. The second round of PCR was conducted in the same manner by using 2.5 µL of the PCR products from the first round PCR reaction as the template. The PCR products were analyzed by using 2% agarose gel electrophoresis and photographed.
Assessing Effects of HPV18 E6 or E7 Targeted RNA Interference in SKBR3 Cells
Constructing shRNA Plasmids and Transfection The target sequences were selected from the HPV18 E6 and HPV18 E7 mRNAs. The target sequence of shE6 (targeting HPV18 E6 nucleotides 301-319) was 5'-TTATTAATAAGGTGCCTGC-3'. The sequence of shE7 (targeting HPV18 E7 nucleotides 82-98) was 5'-CACGAGCAATTAAGCGA-3'. The negative control shRNA sequence (shNC) was 5-'AATATGTTAAG ATACTCGCT-3', which was derived from a randomly reshuffled sequence of HPV18 E7. All the shRNA sequences were confirmed by BLAST to share no homology with any part of the human genome.
Both forward and reverse oligos of shRNA was synthesized, including BglII site (sense of target sequence), Hairpin (antisense of target sequence),and HindIII site. The forward and reverse oligos were annealed and cloned into the vector ρSUPER RNAi System (OligoEngine, Washington, USA) between the unique BglII and HindIII enzyme sites according to the manufacturer's instructions.
To obtain the maximal RNAi effects, the shRNA plasmid transfections were performed following the manufacturer's instruction. Six microliters of the FuGENE® (Promega, Wisconsin, USA) reagent was mixed with 100 µL of OPTI-MEM (Gibco,Massachusetts, USA) and incubated for 5 min at room temperature. Two micrograms of plasmid was then added and the entire mixture was incubated for 15 min at room temperature. The plasmid mixture was then added to the SKBR3 cells (60% confluence). A GFP tag was included in the plasmid to determine the transfection efficiency.
Real-time Quantitative PCR Analysis Total RNA was extracted from the SKBR3 cells 72 h after transfection by using Trizol as described above. The reverse transcription reaction was performed by using the GoScript Reverse Transcription System (Promega, Wisconsin, USA). Real-time quantitative PCR was performed by using the GoTaq qPCR Master Mix (Promega, Wisconsin, USA). The level of mRNA expression was assessed by using the threshold cycle (CT) values. The CT values of the expression levels of genes associated with cell proliferation and apoptosis, such as retinoblastoma (RB), tumor protein p53 mutant (Tp53-mutant), proto-oncogene E3 ubiquitin protein ligase (MDM2), cyclin A1 (CCNA1), cyclin D1 (CCND1), and B-cell CLL/lymphoma 2 (BCL2), were normalized with the expression level of β-actin. Previous studies indicated that the Tp53 mutation was present in the SKBR3 cells. The reaction conditions were 95 °C 10 min; 40 cycles of 95 °C for 15 s and 60 °C for 1 min;then a dissociation stage was added by using the same temperature and time parameters. The level of mRNA expression was quantified in triplicate for every sample. The primer sequences are shown in Table 1.
Analysis of in Vitro Cell Viability, Metastasis, and Growth Cycle Cell viability was assessed with a colorimetric assay by using Celltiter-Glo Luminescent cell viability assay kit (Promega, Wisconsin, USA)according to the manufacturer's instructions. For the colony formation assay, cells were transfected with shRNA, incubated for 48 h, trypsinized, and then seeded in 6-well plates at a concentration of 2500 cells/well. The cells were incubated at 37 °C for 10 days. After washing twice with PBS, the colonies were fixed with 5% paraformaldehyde for 15 min and stained with Giemsa for 10 min. Visible colonies were photographed and counted.
For the cell metastasis analysis, a 24-well permeable support plate (Corning, Massachusetts,USA) was prepared according to the following protocol: the permeable support was covered with 100 µL diluted matrix coating solution (Corning,Massachusetts, USA) at a final concentration of 300 µg/mL then incubated at 37 °C for 2 h. The upper chamber of the plate was inoculated with 2.5×104cells that had been transfected with shRNA,incubated for 48 h, and trypsinized in medium with 2% FBS. The lower chamber contained medium with 20% FBS. After incubation at 37 °C in 5% CO2for 12 h,the lower surface of the membrane was washed,fixed, stained, and observed as described, while the upper surface was cleaned with a cotton swab.
For the cell cycle analysis, cells were transfected with shRNA, incubated for 48 h,trypsinized, and then fixed with ice-cold 70% ethanol at 4 °C for 12 h. The cells were then washed twice with PBS, and resuspended in a PI solution and incubated at 37 °C for 30 min. The samples were analyzed by flow cytometry (Becton, Dickinson and Company, New Jersey, USA).
Statistical Analysis
A one-way ANOVA test was used to examine the association between shRNA and control plasmids with SPSS software version 18.0 (SPSS Inc, IL, USA). All the P-values were two-sided, and the significance level was set at P<0.05.
RESULTS
Detection of HPV Oncogenes in SKBR3 Cells and Breast Cancer Tissue Samples
Detection and Sequencing of HPV Oncogenes in SKBR3 Cells HPV18E6-155 (306-460) and HPV18E7-125 (86-210) were amplified and sequenced from the cDNA of the SKBR3 cells. HPV18E7-100 (80-179) was amplified and sequenced from the DNA of the SKBR3 cells. However, HPV16E6 and HPV16E7 were not detected in the DNA or cDNA of the SKBR3 cells by PCR. The sequence alignment for E6 and E7 with a consensus sequence [Human papillomavirus-18, complete genome (Genebank accession: NC_001357.1)] are shown in Figure 1A and Figure 1B. The sequencing analysis indicated that there was a T→C mutation at 381 bp of HPV18E6-155 (306-460), an A→G mutation at 147 bp of HPV18E7-125 (86-210), and an A→G mutation at 147 bp of HPV18E7-100 (80-179) (Figure 1A). The mutation in HPV18E7-100 (80-179) was the same as the mutation in HPV18E7-125 (86-210) (Figure 1B). None of the mutations resulted in an amino acid change.
Detection of HPV Oncogenes in 76 Paraffinembedded Breast Cancer Samples We then determined whether we could detect HPV oncogenes in primary breast cancer samples with PCR based methods. Eighteen of 76 samples (23.68%)were positive for HPV18 E7 expression by PCR using HPV18E7-100 (80-179) primer. Five of the 76 samples (6.58%) were positive for HPV18 E6 expression by PCR with HPV18E6-322 (66-387)primer. While all the 76 samples were negative for HPV16E6 and HPV16E7 by PCR. Representative results are shown in Figure 2. The sequence alignments of E6 and E7 with a consensus sequence [Human papillomavirus-18, complete genome (Genebank accession: NC_001357.1)] are shown in Figure 3A and Figure 3B. The sequencing analysis indicated that there were deletions and subtle mutations. The tumors were staged by using the TNM staging scale. More tumor samples were HPV18 E7 positive in stage III (61.54%, 8/13) than in stage I (16.67%, 6/36) or stage II (15.38%, 4/26). While more tumor samples were HPV18 E6 positive in stage III (21.43 %, 3/14) than in stage II (8%, 2/25),the differences were not significant. One case of invasive lobular carcinoma was PCR negative for HPV oncogenes.
Assessing Effects of HPV18 E6 or E7 Targeted RNA Interference in SKBR3 Cells
Assessing Effects of HPV18 E6 or E7 shRNA on Cell Cycle Related Proteins in SKBR3 Cells Successful transfection of SKBR3 cells with the shE6 and shE7 shRNA constructs was demonstrated 48 h after transfection by expression of GFP (Figure 4A). Compared with the shNC, the expression levels ofHPV18 E6 and E7 significantly decreased by 34.47% and 78.08% (P<0.05), respectively, after transfection with their respective shRNA (Figure 4B). The expression levels of cell proliferation and apoptosis proteins such as RB, Tp53-mutant, MDM2, CCNA1,CCND1, and BCL2, were evaluated by fluorescent quantitative PCR (Figure 4B). When the shE6 construct was compared with the shNC, the expression of RB significantly increased by 93.86% (P<0.01). In contrast, the expression levels of Tp53-mutant, MDM2, CCNA1, CCND1, and BCL2 significantly decreased by 54.86%, 63.14%, 7.01%,18.48%, and 39.11% (P<0.05). Similarly, when the shE7 construct was compared with the shNC the expression level of RB significantly increased by 100.08% (P<0.01), and the expression levels of Tp53-mutant, MDM2, CCNA1, CCND1, and BCL2 significantly decreased by 39.29%, 36.05%, 15.23%,23.14%, and 76.75%, respectively (P<0.05).
Assessing Effects of HPV18 E6 or E7 shRNA on SKBR3 Viability, Colony Formation,Metastasis,and Cell Cycle Cell viability was examined by a colorimetric assay based on the change of ATP concentration. Forty-eight hours after transfection with targeted shRNA, the viability of the SKBR3 cells was significantly reduced in both the HPV18 E6 and E7 shRNA transfected groups compared with the shNC group (P<0.05; Figure 5). To evaluate the effects on cell colony formation,cells were trypsinized,seeded,and incubated,then stained with crystal violet and counted 48 h after transfection with shRNA. Targeted knockdown of HPV18 E6 and E7 significantly reduced the number of SKBR3 cell colony formation by 60.64% and 63.95%,respectively,compared with the shNC group (P<0.05; Figure 6 A-B). To determine whether HPV18 E6 and E7 were important for the invasive properties of SKBR3 cells, the metastasis abilities of SKBR3 cells transfected with shE6 and shE7 were analyzed in a transwell experiment. Compared with the shNC group, shE6 and shE7 significantly reduced the number of cell metastasis through the polycarbonate membrane by 58.70% and 65.41% (P<0.01; Figure 6C-D), respectively. Flow cytometry was used to analyze the influence of HPV18 E6 or E7 on cell-cycle and apoptosis 48 h after transfection. ShE6 and shE7 significantly increased the percentage of cells in the G0/G1 phase compared with the shNC group (P<0.05). This increase in the number of cells in the G0/G1 phase was coupled with a significant decrease in the percentage of cells in S and G2 phases after 48 h of transfection (P<0.05; Figure 7).
DISCUSSION
The role of HPV in breast cancer is not clearly defined. In this study, HPV18 E6 and E7 gene segments were observed in the mRNA of the SKBR3 cells, and the gene segments of (or similar to) HPV18 E7 were present in the DNA of SKBR3 cells. We also demonstrated that HPV18 E6 and E7 gene segments were also able to detect the presence of HPV in 76 paraffin-embedded breast cancer samples (6.76% and 23.68%). Finally, we also showed that targeted knockdown of HPV18 E6 and E7 using shRNA techniques had an inhibitory effect on breast cancer cell proliferation, metastasis, and cell cycle. These findings suggested that HPV18 E6 and E7 might play an important role in the viral etiology of humanbreast cancer. Importantly, targeted knockdown of HPV18 E6 or E7 might be useful as a potential therapy for breast cancer.
Previous studies have pointed out possible routes for HPV to reach the human breast[13]. Firstly,virus particle in the air could invade through the ducts into the breast tissue directly. Secondly,HPV-infected T-cells and B-cells from the mesenteric lymph nodes or HPV-infected cervical cells might enter the breast tissue via the circulatory system and infect the breast. When the breast tissue becomes infected with HPV, virus particles enter the cell,affecting cell cycle progression and eventually causing breast cancer[18]. There are conflicting reports about the existence of HPV genes in human breast cancer samples and in the SKBR3 cells. Since the first reports about HPV infection caused breast cancer in 1992[19], there have been controversial reports about the etiology of breast cancer around the world[10,14,20-21]. We used primers for HPV oncogenes to screen 76 breast cancer tissue samples from patients. Of these samples, 6.76% were positive for HPV18 E6 and 23.68% were positive for HPV18 E7. We did not find evidence of HPV 16 E6 or E7 in breast cancer samples as same as the results from Mexico[11]and Australia[22]which might be due to the differences in race, primers used, and type of samples[4]. Based on our in vitro results and the outcome of PCR screen, we believe that HPV is associated with human breast cancers. Furthermore,the detection of HPV18 E6 and E7 in multi types of breast cancer suggested that virogene targeted gene therapy would be an effective solution for breast cance.
In regards to SKBR3 cells, Heng et al. described the presence of the HPV18 L1 gene found
with GP5/GP6 primers by PCR and HPV18 E6 by in-situ hybridization[5]. In contrast, Peran et al. screened SKBR3 cells by PCR for HPV18 E6 with two pairs of primer and E7 with one pair of primer by PCR[15]. Given the conflicting data, we chose to use more than 20 pairs of primers for HPV18 E6 or E7 (data not shown). Similar to Heng et al., we also found evidence for HPV18 E6 and E7 gene segments in the mRNA of SKBR3 cells, and HPV18 E7-like gene segments in the DNA of SKBR3 cells[5]. However, we could not confirm the existence of HPV18 E6 in the DNA of the SKBR3 cells because in the PCR analysis,an erroneous band with similar length to the HPV18 E6 product was always present (not show in data).
Most studies pertaining to gene therapy for breast cancer using RNAi technology have focused on human origin genes, such as BCL2[23]and vascular endothelial growth factor A (VEGFA)[24]. Our study has analyzed the development of viral gene therapy in human breast cancer. The knockdown of HPV18 E6 and E7 clearly affected the expression levels of some cell cycle related proteins, such as Tp53-mutant, RB, MDM2, CCDNA1, CCND1, and BCL2. The mRNA expression results of MDM2 and Tp53-mutant were consistent with the flow cytometry results, suggesting that the apoptosis was enhanced or the cell cycle was blocked. The mRNA expression results for CCNA1, CCND1, BCL2, and RB were consistent with the results of viability, colony formation, and cell metastasis assays, indicating that the proliferation of cancer cells was enhanced. These results suggested that HPV18 E6 and E7 might play an important role in the carcinogenic potential of SKBR3 cells and could be used as potential targets for molecular-based therapy for human breast cancer.
Future studies with large sample size are needed to understand the role of HPV in the viral etiology of human breast cancer. Future studies should explore the route of HPV infection in breast cancer and analyze the relationship between HPV infection and breast cancer, and the expression levels of HPV oncogene in relation to human breast cancer.
ACKNOWLEDGEMENTS
We thank the Peking University People´s Hospital for the provision of samples.
Accepted: April 26, 2016
REFERENCES
1. Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin, 2014; 64, 9-29.
2. Lawson JS. Do viruses cause breast cancer? Methods Mol Biol,2009; 471, 421-38.
3. Amarante MK, Watanabe MA. The possible involvement of virus in breast cancer. J Cancer Res Clin Oncol, 2009; 135,329-37.
4. Wang T, Chang P, Wang L, et al. The role of human papillomavirus infection in breast cancer. Med Oncol, 2012; 29,48-55.
5. Heng B, Glenn WK, Ye Y, et al. Human papilloma virus is associated with breast cancer. Br J Cancer, 2009; 101, 1345-50.
6. Zur Hausen H. Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer, 2002; 2, 342-50.
7. Pyeon D, Newton MA, Lambert PF, et al. Fundamental differences in cell cycle deregulation in human papillomaviruspositive and human papillomavirus-negative head/neck and cervical cancers. Cancer Res, 2007; 67, 4605-19.
8. Marur S, D'Souza G, Westra WH, et al. HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol,2010; 11, 781-9.
9. Sigaroodi A, Nadji SA, Naghshvar F, et al. Human papillomavirus is associated with breast cancer in the north part of Iran. Scientific World Journal, 2012; 837191.
10.Akil N, Yasmeen A, Kassab A, et al. High-risk human papillomavirus infections in breast cancer in Syrian women and their association with Id-1 expression: a tissue microarray study. Br J Cancer, 2008; 99, 404-7.
11.Antonsson A, Spurr TP, Chen AC, et al. High prevalence of human papillomaviruses in fresh frozen breast cancer samples. J Med Virol, 2011; 83, 2157-63.
12.Herrera-Romano L, Fernandez-Tamayo N, Gomez-Conde E, et al. Absence of human papillomavirus sequences in epithelial breast cancer in a Mexican female population. Med Oncol,2012; 29, 1515-7.
13.Chang P, Wang T, Yao Q, et al. Absence of human papillomavirus in patients with breast cancer in north-west China. Med Oncol, 2012; 29, 521-5.
14.Hedau S, Kumar U, Hussain S, et al. Breast cancer and human papillomavirus infection: no evidence of HPV etiology of breast cancer in Indian women. BMC Cancer, 2011; 11, 27.
15.Peran I, Riegel A, Dai Y, et al. Is HPV-18 present in human breast cancer cell lines? Br J Cancer, 2010; 102, 1549-51.
16.Fire A, Xu S, Montgomery MK, et al. Potent and specific genetic interference by double-stranded RNA in Caenorhabditis legans. Nature, 1998; 391, 806-11.
17.Liu X, Jiang F, Kalidas S, et al. Dicer-2 and R2D2 coordinately bind siRNA to promote assembly of the siRISC complexes. RNA,2006; 12, 1514-20.
18.Bodaghi S, Wood LV, Roby G, et al. Could human papillomaviruses be spread through blood? J Clin Microbiol,2005; 43, 5428-34.
19.Di Lonardo A, Venuti A, Marcante ML. Human papillomavirus in breast cancer. Breast Cancer Res Treat, 1992; 21, 95-100.
20.Silva RG Jr, da Silva BB. No evidence for an association of human papillomavirus and breast carcinoma. Breast Cancer Res Treat, 2011; 125, 261-4.
21.Lawson JS, Glenn WK, Heng B, et al. Koilocytes indicate a role for human papilloma virus in breast cancer. Br J Cancer, 2009;101, 1351-6.
22.Kan CY, Iacopetta BJ, Lawson JS, et al. Identification of human papillomavirus DNA gene sequences in human breast cancer. Br J Cance, 2005; 93, 946-8.
23.Wang Y, Gao S, Ye WH, et al. Co-delivery of drugs and DNA from cationic core-shell nanoparticles self-assembled from a biodegradable copolymer. Nat Mater, 2006; 5, 791-6.
24.Feng Q, Yu MZ, Wang JC, et al. Synergistic inhibition of breast cancer by co-delivery of VEGF siRNA and paclitaxel via vapreotide-modified core-shell nanoparticles. Biomaterials,2014; 35, 5028-38.
Biomed Environ Sci, 2016; 29(5): 331-339 10.3967/bes2016.043 ISSN: 0895-3988
#Correspondence should be addressed to ZENG Yi, NA, PhD, Professor, Tel: 86-10-63552662, E-mail:zengyicdc@sina.com
Biographical note of the first author: YAN Chen, female, born in 1987, PhD candidate, majoring in oncology.
December 2, 2015;
 Biomedical and Environmental Sciences2016年5期
Biomedical and Environmental Sciences2016年5期
- Biomedical and Environmental Sciences的其它文章
- Development of a Novel PmpD-N ELISA for Chlamydia psittaci Infection*
- Evaluation of Six Recombinant Proteins for Serological Diagnosis of Lyme Borreliosis in China*
- Whole Genome Sequencing and Comparisons of Different Chinese Rabies Virus Lineages Including the First Complete Genome of an Arctic-like Strain in China*
- The Status and Associated Factors of Successful Aging among Older Adults Residing in Longevity Areas in China*
- Cognitive Training in Older Adults with Mild Cognitive Impairment
- Dietary Exposure to Benzyl Butyl Phthalate in China*
